The stunning city of Scottsdale, Arizona will host EDPMA’s 2025 RCM Workshop on December 3 and 4, 2025. This workshop is a focused opportunity to navigate the ever-evolving revenue cycle with confidence. Designed with your time in mind, the event features two half-day sessions to minimize time out of the office while maximizing value. Attendees will gain the latest strategies, best practices and tools to optimize revenue cycle performance and boost financial outcomes.

Author Archive for arobertson
EDPMA Statement in Response to New RAND Study “Strategies for Sustaining Emergency Care in the United States.”
A new report by RAND Health Care, which promotes healthier societies by improving health care systems in the United States and other countries, finds the viability of U.S. hospital-based emergency care in peril, with increasingly complex needs and falling payments for physicians.
Federal law requires anyone who seeks care at an emergency department to be assessed and stabilized, regardless of their ability to pay. U.S. hospital emergency department visits have returned to pre-COVID levels, with 120 to 140 million visits annually.
Emergency departments are experiencing the boarding of patients in emergency department beds, increased patient visit complexity, and a significant increase in uncompensated or undercompensated care from both public and private payors. Reimbursement pressures place physician groups at financial risk, with small independent practices in even greater danger. The result is reduced access to care, extended emergency department wait times, and worse patient outcomes.
The RAND study shows Medicare and Medicaid payments to emergency department physicians fell 3.8% per visit from 2018 to 2022. Payments for commercially insured in-network patient visits dropped by 10.9%, while payments for commercial out-of-network visits dropped by 48% over the period studied.
Mahshid Abir, the report’s lead author and a senior physician policy researcher at RAND, stated:
“Urgent action is needed to sustain hospital emergency departments, which act as a safeguard for patients who use the services and communities that rely on them during a crisis. Unless these challenges are addressed, there is an increasing risk that emergency departments will close, more doctors and nurses will leave emergency medicine, and patients will face even longer waits for care.”
The study recommends policy action to ensure the availability and viability of Emergency Medicine, including:
- Shift the responsibility of collecting patient cost-sharing amounts from providers to insurers for clinical care mandated by EMTALA.
- Direct funding mechanisms that would federally fund Emergency Medicine (e.g., DSH for emergency physicians, HRSA funding to supplement EMTALA-mandated care).
- Increase allowed amounts from government payers.
In response to this study, the Emergency Department Practice Management Association (EDPMA), the nation’s only professional physician trade association focused on the delivery of high-quality, cost-effective care in the emergency department, issued the following statement:
“The Emergency Department is the only medical setting that provides care to all patients, regardless of their ability to pay, making it the critical safety net of the U.S. healthcare system. Yet, as emergency visits and severity continue to rise yearly, payments to physicians decrease, as shown by the RAND study. Without urgent and significant policy changes to support emergency medicine providers, the availability of, and access to, care will decline, wait times will increase, and patient outcomes will worsen—particularly for those in greatest need of care.”
The RAND report, which received support from the Emergency Medicine Policy Institute, is based on interviews and focus groups with emergency medicine professionals, a survey of more than 200 emergency medicine department leaders, case studies, a review of other published research, and analysis of deidentified claims data. The study was overseen by a 13-member advisory board that included emergency medicine professionals, emergency care policy experts, and other health care experts.
For more information on the RAND study, visit www.rand.org.
For EDPMA media inquiries, email Robin Applebaum or Kate Wells.
Save the date for Solutions Summit 2026, taking place at the Wild Dune Resort in Charleston, South Carolina, April 26-29, 2026!
Join us for our upcoming Hill Day, May 6-7, 2025!
May 6: Get briefed on key industry issues and refine your advocacy strategy.
May 7: Meet with Congressional representatives to advance emergency medicine priorities.
Your expertise matters. Join us in Washington, D.C. to network with industry leaders and make a difference.
Interested in attending? Email: [email protected].
Solutions Summit 2025, March 30 – April 2, was an unparalleled educational and networking conference tailored specifically for professionals in emergency medicine.
Solutions Summit is the premier conference dedicated to the business of emergency medicine, featuring in-depth discussions on critical topics such as: the No Surprises Act, reimbursement and regulatory policy, independent dispute resolution, revenue cycle management, and much more!
EDPMA Calls on CMS to Develop State Medicaid Provider Enrollment Reciprocity
The Emergency Department Practice Management Association (EDPMA) is committed to ensuring that patients receive timely access to emergency care no matter when their emergency
happens. This commitment requires the resources necessary to deliver care in our nation’s emergency departments in a sustainable environment – in every state of our union.
Unfortunately, emergency medicine physicians and their clinical practices continue to face unprecedented financial and operational challenges as we address markedly increasing clinical
demands in a setting of well-known health care workforce shortages. The realities of stagnant and declining reimbursement are further complicated by outdated regulatory stipulations that
impose significant administrative burdens.
Click here to read the full statement.
EDPMA Backs New Legislation to Support Patients and Physicians
McLean, VA – The Emergency Department Practice Management Association (EDPMA) is throwing its full support behind newly introduced legislation aimed at supporting timely provider payments by health insurance companies, in order to preserve our nation’s healthcare safety net.
EDPMA has long supported the patient protections in the No Surprises Act (NSA). However, years after the NSA’s implementation, and despite clear requirements in the law itself, health insurance companies are repeatedly failing to pay physicians within 30 days after losing in the independent dispute resolution (IDR) process provided in the law.
Today, a bipartisan group of legislators (Rep. Greg Murphy, M.D. (R-NC), joined by Reps. Ruiz, M.D. (D-CA), Joyce, M.D. (R-PA), Panetta (D-CA), and Schrier, M.D. (D-WA) as original cosponsors), introduced H.R. 9572, The No Surprises Act Enforcement Act. With this legislation, health insurance companies that fail to pay providers in a timely manner after an independent dispute resolution decision will face consequences for ignoring clear statutory obligations. The legislation is designed to reinforce the fair and balanced process that Congress provided in the original No Surprises Act.
Currently, with very limited enforcement and insufficient consequences for health plans that ignore the NSA’s requirements, physician practices continue to feel significant strain from low initial payments and later, from failure of health plans to pay the amounts fairly awarded by an independent arbiter, even though timely payment is required by law.
Since 1987, the Emergency Medical Treatment and Active Labor Act (EMTALA) federal law has required that emergency physicians provide an evaluation and stabilizing treatment for any patient that seeks medical care, regardless of their ability to pay. Under the NSA, if the insurer’s payment for out of network clinical care is inadequate, an emergency physician can dispute the low payment amount through the NSA’s Independent Dispute Resolution process.
When the independent arbiter rules in favor of the physician, the insurer is legally obligated to pay the awarded amount within 30 days. Public data indicates that approximately 80% of the time, independent arbiters have found the physician’s request to be more reasonable than the health plan’s initial payment. However, the additional amounts owed by health plans have not been paid consistently, or have not been paid at all, despite the clear requirements in the law. An April 2024 EDPMA survey about the NSA, members noted that in disputes where the provider was the prevailing party, 24% were still not paid or were paid correctly within the 30 day requirement in the law.
“With this bill, insurance companies that have been exploiting the No Surprises Act will finally be held accountable,” said EDPMA Chair Andrea Brault, MD, FACEP, MMM. “In the Independent dispute resolution process, independent arbiters have agreed that insurers are paying providers inordinately low rates a large majority of the time, which already jeopardizes community-based practices and patient access to care. We support all of the patient protections in the NSA and now, urge Congress to hold health plans accountable for their obligations under the law.”
The proposed legislation, H.R. 9572, will require health plans to pay interest and penalties on unpaid amounts due to providers under the No Surprises Act.
EDPMA urges Congress to pass this bill to ensure that insurance companies pay physicians and their practices fairly and promptly, allowing them to continue providing essential care to their patients.
####
About EDPMA
The Emergency Department Practice Management Association (EDPMA) is the nation’s only professional trade association focused on the delivery of high-quality, cost-effective care in the emergency department. EDPMA’s membership includes emergency medicine physician groups of all sizes, billing, coding, and other professional support organizations that assist healthcare clinicians in our nation’s emergency departments. Together, EDPMA members see or support 60% of all annual emergency department visits in the country. www.edpma.org
Contact:
Cathey Wise, CAE EDPMA Executive Director
817.905.3310
[email protected]
Download the PDF version of this press release here.
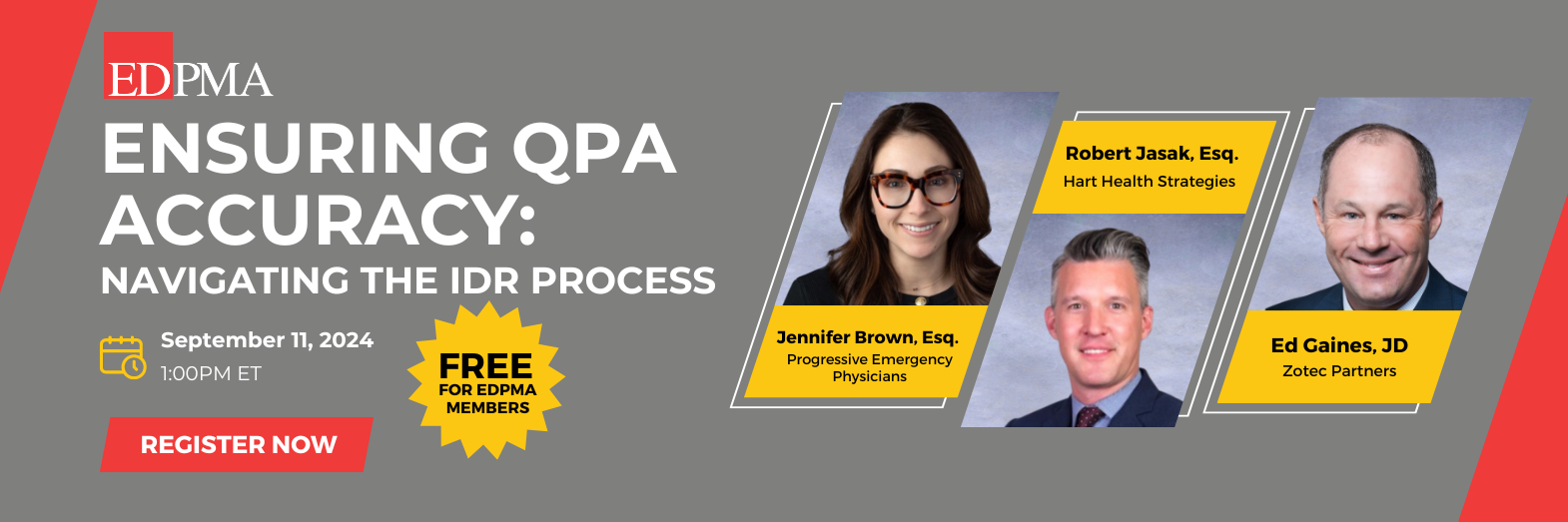
EDPMA members are invited to join us for an exclusive members-only event dedicated to exploring the pivotal role of Qualifying Payment Amounts (QPAs) in the Federal Independent Dispute Resolution (IDR) process. This free event kicks off at 1:00 PM EDT and features a series of discussions led by experts Jennifer Brown, Esq., Robert Jasak, Esq., and Ed Gaines, JD. Through in-depth analysis, we’ll cover the importance of QPAs in cost-sharing determinations, the impact of recent court rulings, and best practices for ensuring QPA accuracy. Gain insights into the regulatory landscape, QPA reliability, and future guidance in this evolving area of healthcare policy. Learn more!
The beautiful The Cosmopolitan in Las Vegas hosted EDPMA’s annual RCM Workshop on December 10 and 11. This workshop will give you the “Revenue Rendezvous” needed to help you navigate the revenue cycle! This conference includes (2) half-day sessions (to minimize your time out of the office) and will equip you with the latest strategies, best practices, and tools to optimize your revenue cycle and enhance overall financial performance.
Our Pre-Conference Session is BACK! This half-day session will help you understand the impact lawsuits are having on the regulations, learn how EDPMA’s No Surprises Act I-Tact Committee and advocacy with CMS & CCIIO informed and impacted improved health plan compliance and the IDR process in general and ask questions from an expert panel.
December 10-11, 2024 | The Cosmopolitan, Las Vegas, NV
EDPMA Virtual Workshop: Value-Based Contracting – From Concepts to Reality
Join us for an EDPMA Virtual Workshop!
- Date: September 4, 2024
- Time: 1pm – 4pm ET
- Location: Zoom (link to be sent upon registration)
What This Workshop Will Cover:
In recent years, health care entities have deployed significant efforts to transform fee-for-service payment into value-based models of care. However, emergency medicine practices have not been proportionately included in these efforts, despite data and experiences that repeatedly reveal substantial opportunities to impact quality, outcomes, and cost that are essential to the success of value-based models.
Value-based models can take many forms, with considerable ranges of risk, opportunity, required investments, and clinical/operational demands. In recent years, some emergency medicine practices have created and deployed value-based models. Increasingly, there are common themes and metrics of interest including quality measures, avoidable hospitalizations, reducing ED bounce-backs, and addressing variation in clinical decision-making. Positive outcomes have resulted.
For many practices however, it is difficult to know where to start, how to proceed, and how to establish and deploy a value-based model. This Workshop is an interactive session that provides background, information, and tools to empower your group’s value-based journey. Experienced experts will share their own journey, their results, and lessons learned. And interactive breakout sessions will enhance your learning experience with interested colleagues in our specialty.
Randy Pilgrim, MD, FACEP, FAAFP will provide a brief review of Value-Based Care (VBC) concepts for emergency medicine, fundamental program types, and examples of successful programs currently in practice.
Lisa Mauer, MD will describe a process designed to activate your relationships and local market awareness into profitable, winning contracts. We will break into groups to evaluate current situations that offer potential for VBC, including:
- Establishing contacts
- Identifying and assessing opportunities
- Defining the program
- Winning the contract
- Implementation
Jesse Pines, MD will cover the fundamentals of measurement, benchmarking, and using data analytics to change behavior through a virtuous cycle of measure-improve-measure-improve, where success naturally leads to new, more lucrative VBC opportunities.
Lastly, our expert panel will lead a discussion entitled “Now What” to help energize our group of leaders to confidently pursue better contracts tied to value starting now!
Our Workshop Faculty:
- Randy Pilgrim, MD, FACEP, FAAFP – Enterprise Chief Medical Officer, SCP Health
- Lisa Mauer, MD – Chief Medical Officer, ConsensioHealth
- Jesse Pines, MD – Chief of Clinical Innovation, US Acute Care Solutions
Pricing:
Individual Member: $400
Individual Non-Member: $500
Member Group Registration (3 or more from one organization): $1,100
Non-Member Group Registration (3 or more from one organization): $1,400
For all group registrations, please contact [email protected] to register your entire group. When you register as a group, you must be registered all at once and pay with a single form of payment.
If you are with a member organization and you see the non-member price, you are not on your organization’s roster, please see your organization’s admin. Your organization administrator can add you to the roster with these simple steps.
